procedures
Colonoscopy
WHAT YOU SHOULD KNOW ABOUT COLONOSCOPY
What is a colonoscopy?

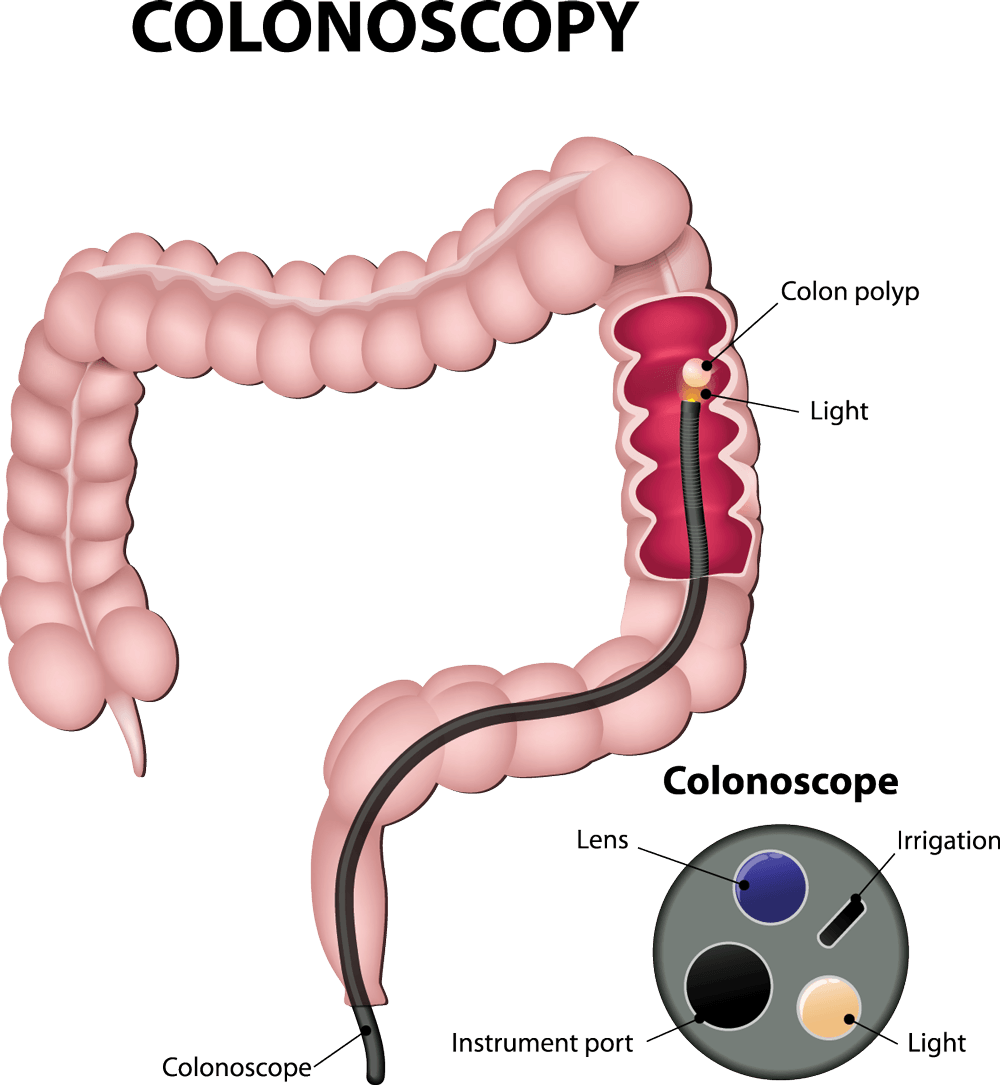
A colonoscopy lets your doctor examine the lining of your large intestine or colon for abnormalities by inserting a thin. flexible tube into your anus and slowly advancing it into your rectum and colon. This instrument, a colonoscope, allows your doctor to view images on a video monitor.
Why is a colonoscopy recommended?
Colonoscopy can screen for colorectal cancer, the third leading cause of cancer deaths in the US. Annually, about 150,000 new cases of colorectal cancer are diagnosed in the US and 50,000 people die from the disease. Increased awareness and screening would save at least 30,000 lives each year. Your doctor may also recommend the exam to evaluate symptoms such as bleeding and chronic diarrhea.
What preparations are required?
Your doctor will tell you what dietary restrictions to follow and what cleansing routine to use. In general, the prep consists of drinking clear liquids the day before and consuming a special cleansing solution or oral laxatives. Your colon must be completely clean for the procedure to be accurate and comprehensive, so follow instructions carefully.
What happens during a colonoscopy?
A colonoscopy rarely causes much pain. You might feel pressure, bloating or cramping during the procedure. Typically, your doctor will give you a sedative or painkiller to help you relax and better tolerate any discomfort.
You will lie on your side or back while your doctor slowly advances a colonoscope through your large intestine to examine the lining. Your doctor will examine the lining again as they withdraw the colonoscope. The procedure usually takes less than 45 minutes, but plan on two to three hours for waiting, preparation and recovery.
In some cases, your doctor cannot pass the colonoscope through your entire colon to where it meets the small intestine. Your doctor will advise you whether any additional testing is necessary.
What if the colonoscopy shows something abnormal?
If your doctor thinks an area needs further evaluation, they might pass an instrument through the colonoscope to obtain a biopsy - a small sample of the colon lining - for analysis. Biopsies are used to identify many conditions, and your doctor will often take a biopsy even if they don't suspect cancer.
If the colonoscopy is done to identify sites of bleeding, your doctor might control the bleeding through the colonoscope by injecting medications, cauterizing or sealing off vessels with heat treatment, or using small clips. Your doctor might also find polyps and will probably remove them during the exam. These procedures usually don't cause any pain.
What are polyps and why are they removed?
Polyps are abnormal growths in your colon lining that are usually benign - not cancerous. They vary in size from a tiny dot to several inches. Your doctor cannot tell a benign polyp from a cancerous one by its appearance, so they will remove them for analysis. Because cancer begins in polyps, removing them is an important way to prevent colorectal cancer.
How are polyps removed?
Your doctor will remove polyps by using wire loops called snares or biopsy instruments. These instuments are passed through the colonoscope and can be used with or without electrical current. You should feel no pain during the polypectomy.
What happens after a colonoscopy?
You will be monitored until most of the effects of the anesthesia have worn off. You might have some cramping or bloating because of the air introduced into your colon during the exam.
This should disappear fairly quickly when you pass gas.
Your physician will explain the results to you, although you will have to wait for the results of any biopsies. If you have received anesthesia, someone must drive you home and stay with you. Even if you feel alert after the procedure, your judgment and reflexes could be impaired for the rest of the day.
You should be able to eat after the exam, but your doctor might restrict your diet and activities, especially after a polypectomy.
What are possible complications?
Colonoscopy and polypectomy are generally safe when performed by doctors specially trained and experienced in these procedures. One possible complication is a tear through your bowel wall that could require surgery. Bleeding might occur at the biopsy or polypectomy site, but it's usually minor. Bleeding can stop on its own or be controlled through the colonoscope. Some patients might have a reaction to the sedatives anesthesia or complications from heart or lung disease. Although complications after colonoscopy are uncommon, contact your doctor if you notice severe abdominal pain, fever and chills, or rectal bleeding. Note that bleeding can occur several days after the procedure.